Current Issue
Rate of Art Adherence and Clinical Outcome Among HIV Patients with Opportunistic Infection in an Urban Hospital in Eastern DRC
Olivier Mulisya1,*, Franck Katembo Sikakulya2, Adam Moyosore Afodun3, Simon B Mambo4, Dalton Kambale Munyambalu5, David Wol Nang6, Justine Musubao Vuma2
1Department of Gynecology and Obstetrics, Université de Conservation de la Nature et de Développement de Kasugho, GOMA, DRC
2Faculty of Medecine, Université Catholique du Graben, Butembo, DRC
3Department of Anatomy and Cell Biology, Faculty of Health Sciences, Busitema University, Uganda
4Department of Public Health, School of Allied Health Sciences, Kampala International University, Ishaka, Uganda
5Department of Internal Medicine, Kampala International University-Teaching Hospital, Bushenyi, Uganda
6Department of Obstetrics and Gynecology, Kampala International University Teaching Hospital, Ishaka-Bushenyi, Uganda
*Corresponding author: Olivier Mulisya, Department of Gynecology and Obstetrics, FEPSI Hospital Butembo, DRC , Phone: 243997719443, E-mail: olimulisya@yahoo.fr
Received Date: September 02, 2024
Publication Date: October 25, 2024
Citation: Mulisya O, et al. (2024). Rate of Art Adherence and Clinical Outcome Among HIV Patients with Opportunistic Infection in an Urban Hospital in Eastern DRC. Clin Res. 5(1):25.
Copyright: Mulisya O, et al. © (2024).
ABSTRACT Background: In low- and middle-income countries (LMICs), the global rollout of highly active antiretroviral therapy (HA+ART) has led to a decline in HIV-related deaths. However, Loss to follow-up (LTFU) is a significant cause for treatment failure and threatens the enhancement of HIV treatment outcomes among patients on ART. The aim of this study was to determine the rate of ARV adherence and clinical outcome among HIV patients with opportunistic infections attending an urban hospital in Eastern Democratic Republic of the Congo. Methods: We conducted a cross-sectional study for 6 months, from May to December 2022 at FEPSI Hospital in Butembo city. All HIV patients presenting with opportunistic infections diagnosed and managed at this hospital were consecutively enrolled. Stratified questionnaires were used to collect participant characteristics. Descriptive statistics followed by binary logistic regression were conducted using SPSS version 26, and a p≤0.05 was considered statistically significant at 95% confident interval. Results: The rate of ARV adherence was 27.87% while the mortality rate was 25.41% among HIV patients with opportunistic infections. On multivariate logistic regression, not adhering to HIV medicine (aOR=19.885, CI:3.661-108.012, p=0.001), non-ambulating (supine positon) on admission (aOR=26.982, CI:3.234-225.140, p=0.002) were found to be independently associated with mortality among HIV patients. Conclusion: Among HIV patients with opportunistic infections in our setting, the rate of ARV adherence is still low while the mortality rate remains high. Hence, LTFU remains a major factor halting the progress of the prevention and treatment of HIV patients. This study recommends Improving comprehensive counselling services, follow-up for adverse reactions and introducing an ART outcome evaluation program may help reduce LTFU to an acceptable level.
Keywords: Rate of Art Adherence, Clinical Outcome, Opportunistic Infection, Urban Hospital in Eastern DRC
BACKGROUND
Acquired immunodeficiency syndrome (AIDS) has become a major global public health problem [1]. The impact of the introduction of highly active antiretroviral therapy ((HA+ART). The incidence and mortality of human immunodeficiency virus (HIV)-associated opportunistic infections (OIs) has been well documented in high-income countries (HICs). In low- and middle-income countries (LMICs), the global rollout of ART has led to more than 15 million patients on ART, and a decline in HIV-related deaths by 40% since 2004 [2]. In 2012, 9.7 million people received ART in low- and middle-income countries (LMICs) [1], and as of 2013, ART prevented an estimated 4.2 million deaths in LMICs in 2002-2012 [3]. The decline in morbidity and mortality in HIV/AIDS patients coincides with the availability of highly active antiretroviral therapy HA+ART). The advent of antiretroviral therapy (ART) reduces viral replication, increases the number of CD4 lymphocytes and improves their function, re-establishing the defenses of the host and improving chances of survival [4,5].
HIV-positive patients need to use ARVs for life to boost their immune system in order to prevent acquiring opportunistic infections that cause death due to HIV/AIDS manifestations, and to reduce the transmission rate to their partners [5]. Antiretroviral therapy is an intervention to control HIV infection, improving the quality of life and prolonging the survival status of HIV patients. Therefore, discontinuation of ART care and treatment threatened the effectiveness of such interventions [6].
Loss to follow-up (LTFU) is a serious public health concern throughout the world [6]. The LTFU visits is defined as HIV/AIDS not taking ART to refill for a period of 3 months or longer from the last attendance while the patient is not yet classified as “dead” or “transferred-out” [5]. LTFU is a significant cause of treatment failure and threatens the enhancement of HIV treatment outcomes among patients on ART [6]. The WHO proposed the goal of 90-90-90 to ensure that 90% of patients are aware of their disease, 90% receive sustained ART, and 90% of these patients achieve undetectable viral suppression. Nevertheless, LTFU is a serious obstacle to achieving this goal [7].
The impact of regular follow-up is substantial, as even patients returning to care after LTFU might be five times more likely to die from the disease [7]. Given the magnitude of the problem and the fact that no study has been done to date in our area of war where the movement of the population linked to the war would be a factor of loss to follow-up, and given that the FEPSI Hospital is one of the health care providers for HIV patients in this deadly region of eastern DRC, a study evaluating the problem of ARV adherence and clinical outcome among HIV patients with opportunistic infections attending this hospital would be critical in providing local data on this major issue.
METHODS
Study design and area
This was a cross-sectional study conducted at FEPSI Hospital in Butembo city in the Eastern Democratic Republic of the Congo among newly and known HIV patients who sought care in this study area. This centre was chosen based on the fact that it is a known centre for the screening and management of HIV patients in Butembo city.
Study participants, inclusion and exclusion criteria
FEPSI hospital manages an average of 900 patients with HIV. Therefore, we included in this study all HIV patients presenting with opportunistic infections diagnosed and managed at this hospital. The sample size was not determined, as we based our sampling on a consecutive sampling technique whereby all patients presenting signs and symptoms mimicking opportunistic infections who were diagnosed and managed for this purpose were included. We excluded patients with opportunistic infections who were transferred by their willing or their care takers after diagnosis. We assured that all patients included in this study were informed and consented to participate in this study.
Data collection and instrument
The study was conducted for a period of 6 months, from May to December 2022. Assistant researchers (one medical officer and one nurse) were trained on how to conduct data collection. A stratified questionnaire was composed of 11 items developed based on a published paper by Salema et al. (5) and focused on several key constructs: six questions related to sociodemographic characteristics (gender, age, location, education level, occupation and marital status) and five questions related to the clinic presentations of the patients, including the type of OI, consciousness level at admission, position at admission, adherence to HIV medicine and outcome of patients who were managed for OI at Fepsi Hospital. The questionnaire used was made in English and then translated into French by the authors (OM and FKS) before its use.
Data analysis
The raw data were cleaned and entered into Microsoft Excel and exported into SPSS version 26 for statistical analysis. A univariate analysis of all social demographic characteristics of the respondents was performed using the chi-square test, and we presented them in tables and graphics as frequencies and percentages for categorical variables and means and standard deviations for continuous variables. Binary regression analysis to study factors associated with death among HIV patients with OI was performed and presented with the corresponding ORs, 95% CIs, and P values. Variables with a p value<0.2 in bivariate analysis were considered for multivariate analysis.
Ethics
Ethical clearance for the study was obtained from the management of FEPSI Hospital and informed consent of respondents before enrolling them voluntarily in the study. Ethics issues such as privacy and confidentiality of the respondents were ensured. No names or contact information was obtained from the participants.
RESULTS
Characteristics of the study population
The mean age of the study participants we enrolled was 37±13.90; minimum age: 4 and maximum age: 66 (Table 1). The majority of these were female (65.6%), elderly (44.3%), from urban areas (85.2%), not married (77.9%), and had a primary level of education (53.3%).
The rate of ARV adherence
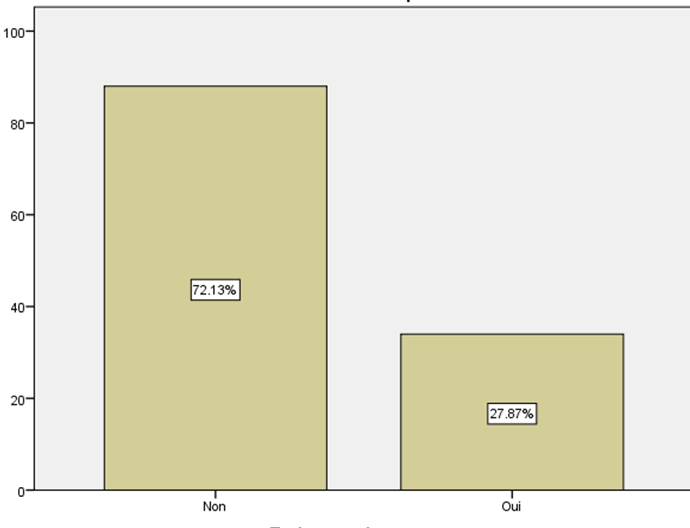
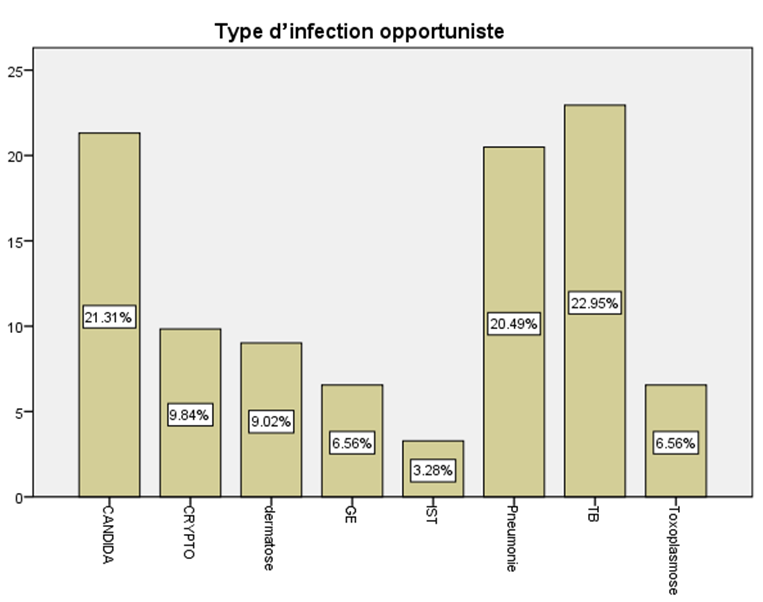
Among the 122 patients enrolled, 34/122 reported adherence to ART; hence The rate of ARV adherence was 27.87% among HIV patients with opportunistic infections (Figure 1). The most common opportunistic infections among the participants were; Tuberculosis, pneumonia and Candida among others (Figure 2).
Clinical outcome among the study participants
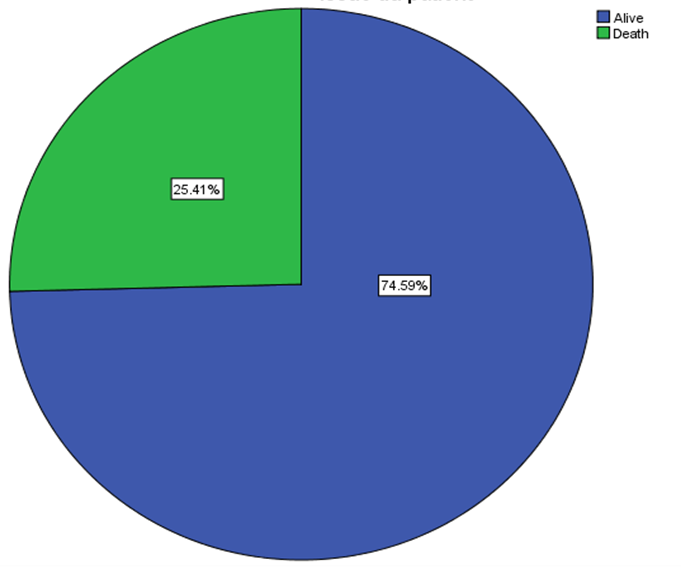
Out of the 122 patients, the overall survival was determined from the time of admission. Overall, 31/122 patients died while 91/122 patients survived. Hence, the mortality rate at admission among HIV patients with opportunistic infections was 25.41% (Figure 3).
Factors associated with mortality among the study participants
Chi-squared sociodemographic (Table 2) rendering displayed heterogeneity in results and suggests the effects of adherence to HIV medicine p< 0.001 is a significant co-factor (among others) to ultimately influence HIV management (table 2). As shown in (Table 3), on binary regression analysis to evaluate factors correlating with death among HIV patients (patient status/position at admission; COR 31.000, bivariate 95% CI 6.923- 138.822, p < 0.001), while unemployment ranked low (COR 1.467, bivariate 95% CI 0.286-7.528, p 0.646) and female gender (COR 0.467, bivariate 95% CI 0.182- 1.197, p 0.113) is particularly susceptible. Marital status (unmarried n=95) directly correlated with approximately 77.9% of experimental cases, with a rate of transmission averaging 26% in our epidemiological studies. On multivariate logistic regression (table 3), not adhering to HIV medicine (aOR=19.885, CI:3.661-108.012, p=0.001), non-ambulatory (supine positon on admission (aOR=26.982, CI:3.234-225.140, p=0.002) were found to be independently associated with mortality among HIV patients.
Table 1. Sociodemographic characteristics
|
Variables |
Options |
Effective, n (122) |
% |
|
Gender |
Male |
42 |
34.4 |
|
Female |
80 |
65.6 |
|
|
Age group |
Under 20 |
15 |
12.3 |
|
21-40 |
53 |
43.4 |
|
|
41 and elder |
54 |
44.3 |
|
|
Location |
Urban |
104 |
85.2 |
|
Rural |
18 |
14.8 |
|
|
Education level |
Sec+Above |
26 |
21.3 |
|
Not schooled |
31 |
25.4 |
|
|
Primary |
65 |
53.3 |
|
|
Occupation |
Unemployed |
14 |
11.5 |
|
House wife |
52 |
42.6 |
|
|
Employer |
56 |
45.9 |
|
|
Marital status |
Married |
27 |
22.1 |
|
Unmarried |
95 |
77.9 |
Figure 1. Rate of HIV medicine adherence among HIV patients with OI.
Figure 2. Opportunistic infections among HIV/AIDS patients at FEPSI Hospital.
Figure 3. Outcome of HIV patients with OI.
Table 2. Chi-squared of sociodemographic, clinic characteristics of HIV patients with OI by outcome
|
Variables |
Alive |
Death |
Total |
p value |
|
|
Gender |
Male |
35(83.3) |
7(16.7) |
42(100.0) |
0.108 |
|
Female |
56(70.0) |
24(30.0) |
80(100.0) |
||
|
Location |
Urban |
78(75.0) |
26(25.0) |
104(100.0) |
0.803 |
|
Rural |
13(72.2) |
5(27.8) |
18(100.0) |
||
|
Occupation |
Unemployed |
12(85.7) |
2(14.3) |
14(100.0) |
0.121 |
|
House wife |
34(65.4) |
18(34.6) |
52(100.0) |
||
|
Employed |
45(80.4) |
11(19.6) |
56(100.0) |
||
|
Education level |
Sec+Above |
22(84.6) |
4(15.4) |
26(100.0) |
0.339 |
|
Primary |
48(73.8) |
17(26.2) |
65(100.0) |
||
|
Not schooled |
21(67.7) |
10(32.3) |
31(100.0) |
||
|
Marital status |
Unmarried |
72(75.8) |
23(24.2) |
95(100.0) |
0.568 |
|
Married |
19(70.4) |
8(29.6) |
27(100.0) |
||
|
HIV Status |
Not known |
24(82.8) |
5(17.2) |
29(100.0) |
0.247 |
|
Known |
67(72.0) |
26(28.0) |
93(100.0) |
||
|
Comorbidity |
Yes |
44(64.7) |
24(35.3) |
68(100.0) |
0.005 |
|
No |
47(87.0) |
7(13.0) |
54(100.0) |
||
|
Adherence to HIV medicine |
Yes |
15(44.1) |
19(55.9) |
34(100.0) |
<0.001 |
|
No |
76(86.4) |
12(13.6) |
88(100.0) |
||
|
Conscious level at admission |
Alert |
85(84.2) |
16(15.8) |
101(100.0) |
<0.001 |
|
Coma |
6(28.6) |
15(71.4) |
21(100.0) |
||
|
Position at admission |
Ambulating |
62(96.9) |
2(3.1) |
64(100.0) |
<0.001 |
|
Supine |
29(50.0) |
29(50.0) |
58(100.0) |
Table 3. Binary regression analysis of factors associated with death among HIV patients with OI
|
Variables |
Options |
Bivariate |
p value |
Multivariate |
p value |
||
|
COR |
95% C.I |
AOR |
95% C.I |
||||
|
Gender |
Male |
1 |
- |
- |
1 |
- |
- |
|
Female |
0.467 |
0.182-1.197 |
0.113 |
2.225 |
0316-15.673 |
0.422 |
|
|
Location |
Urban |
1 |
- |
- |
|||
|
Rural |
0.867 |
0.282-2.664 |
0.803 |
||||
|
Occupation |
Employed |
1 |
- |
- |
1 |
- |
- |
|
Unemployed |
1.467 |
0.286-7.528 |
0.646 |
- |
- |
- |
|
|
House wife |
3.176 |
0.640-15.769 |
0.157 |
0.261 |
0.011-6.277 |
0.408 |
|
|
Education level |
Sec+Above |
1 |
- |
- |
|||
|
Not schooling |
2.619 |
0.710-9.655 |
0.148 |
0.357 |
0.016-7.851 |
0.513 |
|
|
Primary |
1.948 |
0.586-6.470 |
0.276 |
||||
|
Marital status |
Married |
1 |
- |
- |
|||
|
Single |
1.318 |
0.510-3.409 |
0.569 |
||||
|
HIV status |
Known |
1 |
- |
- |
|||
|
Not known |
1.863 |
0.642-5.401 |
0.252 |
||||
|
Comorbidity |
No |
1 |
- |
- |
1 |
- |
- |
|
Yes |
3.662 |
1.435-9.347 |
0.007 |
0.199 |
0.023-1.752 |
0.146 |
|
|
Adherence to HIV medicine |
Yes |
1 |
- |
- |
1 |
- |
- |
|
No |
8.022 |
3.228- 19.939 |
<0.001 |
19.885 |
3.661-108.012 |
0.001 |
|
|
Conscious level at admission |
Alert |
1 |
- |
- |
1 |
- |
- |
|
Coma |
13.281 |
4.479-39.385 |
<0.001 |
3.02 |
0.570-15.993 |
0.194 |
|
|
Position at admission/Patient status |
Ambulanting (Outpatients) |
1 |
- |
- |
1 |
- |
- |
|
Supine (in patients) |
31 |
6.923-138.822 |
<0.001 |
26.982 |
3.234-225-140 |
0.002 |
|
DISCUSSION
The loss of follow-up visits among HIV-positive adults is a leading cause of an increase in HIV morbidity and mortality. In Sub-Saharan African countries, positive clients who were lost to follow-up visits do increase the risk of opportunistic infections due to high viral load and low CD4 count, hence causing death to people with HIV/AIDS [5].
In this study, no adherence to HIV medicine due to loss of follow-up was strongly associated with mortality. Other studies have shown that patients who discontinued ART developed a rapid increase in viral load and depletion of CD4 T lymphocytes, putting them at risk of opportunistic infections and early death [3].
The mortality rate among patients with OI was high in our study. The loss of follow-up visits among HIV-positive adults and those on antiretroviral therapy is a leading cause of morbidity and mortality in Tanzania. The loss of follow-up visits brings a major challenge in the Care and Treatment Centre (CTC), as many HIV clients are not attending clinics as scheduled.
Retention in an antiretroviral clinic has been recognized as an important element of HIV care. Without retention of HIV patients in clinics, the loss to follow-up visit rate will increase morbidity and mortality and drug resistance among HIV/AIDS patients [5]. In Malawi, the loss of follow-up visits was associated with death, whereby HIV patients died and no information was given to the CTC from relatives; hence, the patient was termed lost to follow-up visits [5]. Loss to follow-up (LTFU) negatively impacts the immunological benefit of ART and increases AIDS-related morbidity, mortality, and hospitalizations [3].
Adherence to ART is associated with effects in reducing incidence rates of the loss of follow-up visits and opportunistic infections. This has resulted in a reduction in the number and duration of hospital stays associated with infectious events and mortality rates among people living with HIV/AIDS [5]. In our study, patients who interrupted treatment on ART were likely to die.
However, apart from very little documented evidence about the loss of follow-up visits among HIV-positive adults, more data and studies are still needed to inform policy makers [5].
CONCLUSION
Our findings indicate that, among HIV patients with opportunistic infections in our setting, the rate of ARV adherence is still low while the mortality rate remains high as compared to the global standard. Pulmonary tuberculosis is the most common opportunistic infection and the leading cause of death in HIV-infected patients, followed pneumonia and Candida among other infections. The factors independently associated with increased mortality were; not adhering to HIV medicine and non-ambulatory position. We recommend that consideration should be given to early screening and treatment of OIs. In addition, adherence support through phone calls and case managers could be strengthened to mitigate loss to follow-up by addressing the identified risk factors. Therefore, available intervention modalities should be strengthened.
ABBREVIATIONS
AIDS: Acquired Immunodeficiency Syndrome; ART: Antiretroviral Therapy.
ACKNOWLEDGMENTS
We would like to especially thank the study participants and the entire team. We would also like to thank the ART teams at the study sites for their dedication and support, Saiba Katembo Noella Linga, Gertrude Tambavira.
COMPETING INTERESTS
The author(s) declare that they have no competing interests.
AUTHORS' CONTRIBUTIONS
Dr Olivier Mulisya: Developed protocol, coordinated data collection, conducted data analysis and drafted the manuscript. Dr Franck Sikakulya: Participated in study design, conducted data analysis and supervised data collection. Dr Dalton Kambale Munyambalu participated in the study design and analysis. Dr Simon B Mambo: Advised on study design and analysis. Dr Adam Moyosore: Supervised study design. Dr Justine Musubao Vuma and Dr David Wol Nang participated in drafting and proof reading the manuscript. All authors participated in critical appraisal and revision of the manuscript. All authors have given final approval of the version to be published.
REFERENCES
- Meng S, Tang Q, Xie Z, Wu N, Qin Y, Chen R, et al. (2023). Spectrum and mortality of opportunistic infections among HIV/AIDS patients in southwestern China. Eur J Clin Microbiol Infect Dis. 42(1):113-120.
- Low A, Gavriilidis G, Larke N, B-Lajoie MR, Drouin O, Stover J, et al. (2016). Incidence of Opportunistic Infections and the Impact of Antiretroviral Therapy Among HIV-Infected Adults in Low- and Middle-Income Countries: A Systematic Review and Meta-analysis. Clin Infect Dis. 62(12):1595-1603.
- Megerso A, Garoma S, Eticha T, Workineh T, Daba S, Tarekegn M, et al. (2016). Predictors of loss to follow-up in antiretroviral treatment for adult patients in the Oromia region, Ethiopia. HIV AIDS (Auckl). 8:83-92.
- Dereje N, Moges K, Nigatu Y, Holland R. (2019). Prevalence And Predictors Of Opportunistic Infections Among HIV Positive Adults On Antiretroviral Therapy (On-ART) Versus Pre-ART In Addis Ababa, Ethiopia: A Comparative Cross-Sectional Study. HIV AIDS (Auckl). 11:229-237.
- Salema J. (2015). Factors and Challenges Associated with Loss of Follow up Visits among HIV and AIDS Clients Attending Antiretroviral Therapy in Ilala Municipal Council. Masters’ Thesis, Mzumbe University, Dar es Salaam.
- Birhanu MY, Leshargie CT, Alebel A, Wagnew F, Siferih M, Gebre T, et al. (2020). Incidence and predictors of loss to follow-up among HIV-positive adults in northwest Ethiopia: a retrospective cohort study. Tropical medicine and health. 48:1-10.
- Seyed Alinaghi S, Karimi A, Barzegary A, Pashaei Z, Zargari G, Kianzad S, et al. (2022). Prevalence and reasons of loss to follow-up in HIV clinics: a systematic review of current evidence. HIV AIDS Rev. 21(3):179-190.
 Abstract
Abstract  PDF
PDF